Thyroid antibodies, and figuring out if you can (and should) lower them, is a complex topic that deserves an understandable answer. So, today, I want to help you do exactly that.
In this article, we’ll cover the most pressing questions when it comes to thyroid antibodies: Is it important to lower them? Will it heal your thyroid? Who should lower them? I hope you’ll join me as I explore each of these questions, and many more, in the article below.
Product Recommendation: Dr. Christianson’s New Thyroid Antibody Support Supplement!!! Antibody Support is a thyroid-specific formulation made to reduce the thyroid antibodies found in Hashimoto’s Thyroiditis and Graves’ Disease. Click Here
Thyroid Antibodies: The Quick Summary
Ready for the quick rundown? Here are the most important things you need to know:- Both antithyroglobulin or antithyroid peroxidase levels over 500 IU/mL may be significant
- When they are high your thyroid is more likely to shut down
- This can lead to symptoms like infertility, amongst others
- The most powerful ways to lower antibodies include:
- Iodine regulation
- Weight loss
- Selenium, inositol, and nigella
What Are Thyroid Antibodies?
Antibodies
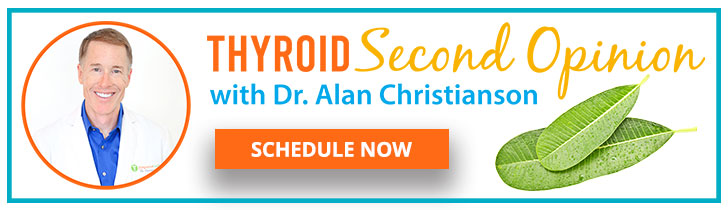
Antibodies are immune proteins that are also called immunoglobulins. They are shaped like the letter Y and are produced in order to help the immune system know what to attack. Different antibodies are made to attach to proteins from something harmful like a virus or a bacteria.
The foreign substance has proteins unique to it called antigens. Antibodies fit with specific antigens (proteins) like a lock fits specific keys. The antibody itself may slow down the foreign organism, but the main thing that it does is shows the rest of your immune system where trouble is lurking.
Autoantibodies
The immune system is not perfect, and sometimes it makes mistakes. Autoantibodies are what we made against our own tissues. This is often for reasons that are not always clear, and people can even have autoantibodies that never cause problems (or cause a lot of them).Thyroid autoantibodies
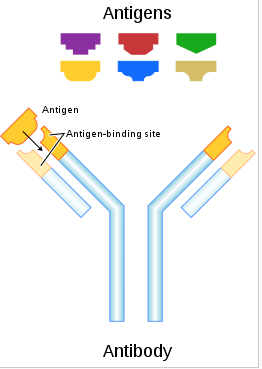
The thyroid makes thyroid hormone by connecting iodine and thyroglobulin (also called Tg for short). Iodine enters the body in a form called iodide. Iodide by itself is not very reactive, so the thyroid uses the enzyme thyroid peroxidase (TPO) to oxidize iodide into iodine. Iodine is highly reactive and easily attaches to thyroglobulin. This is the step in the image below called iodination. Iodine is reactive and releases lots of free radicals. Your thyroid has to make large amounts of antioxidants to protect itself from them.
The long string with the buds coming out of it is thyroglobulin. A full molecule of it has room for 11-13 iodine atoms. When your body has too much iodine, as many as 60 can be stuck on each molecule of thyroglobulin.
This extra iodine might make more free radicals than the thyroid can handle. It can also cause your immune system to think that thyroglobulin is foreign. These processes can cause the body to attack thyroid peroxidase and thyroglobulin.
How Do We Refer To Antibodies?
Sometimes, medical terms are more confusing than helpful. So, here are various ways that you might see thyroid antibodies labeled:- Antithyroidperoxidase = TPO Ab = anti TPO = -TPO = TPO antibodies = thyroid peroxidase antibodies
- Antithyroglobulin = Tb Ab = anti Tg = -Tg = Tg antibodies = thyroglobulin antibodies
Can You Have Hashimoto’s Without Antibodies?
Do you have hypothyroidism but not Hashimoto’s disease? How do you know you don’t have Hashimoto’s? Doctors often tell people they do not have Hashimoto’s simply because they do not have positive thyroid antibodies. Once you realize that thyroid antibodies are only part of the culprit behind thyroid disease, it makes sense that many people with Hashimoto’s do not have positive thyroid antibodies2. There’s a much larger story at play here, and one we need to discover.How Do You Test Your Thyroid Antibodies?
The key types of thyroid antibodies include:- TPO-Ab, Tg-Ab
- Thyroid Stimulating Immunoglobulin (TSI)
- Thyrotropin Receptor Antibodies (TRAb)
- For those suspected of Hashimoto’s, it is best to test TPO-Ab and Tg-Ab
- For those suspected of Graves’, it is also helpful to test TSI
When Should You Test Your Thyroid Antibodies?
First and foremost, it is best to avoid all supplements for three days prior to having thyroid blood tests. This is because supplements, like probiotics and those with biotin, can skew the results. Other thyroid levels can be skewed by additional factors, including the time of day, a recent meal, prior thyroid medications, and the timing of one’s menstrual cycle. In short, the most accurate way to do thyroid tests is to always do them:- Before taking any thyroid medication
- Before food
- Between 6-9 AM
- Three days after taking any supplements
- Between days 1-9 or 21-28 of the menstrual cycle. Not between days 10-20
Is It Important To Lower Your Thyroid Antibodies?
The answer is a thoughtful “maybe.” If your antibodies are both under 100 IU/mL, you have no symptoms, and your thyroid levels are stable, it is probably not worth worrying about your antibodies. On the other hand, you should look to lower them if:- Your TSH is stable, and
- Both of your antibodies are well over 1000 IU/mL, and
- You still have unexplained symptoms like fatigue, joint pain, muscle pain, dry eyes, and poor sleep
High Or Low Antibodies
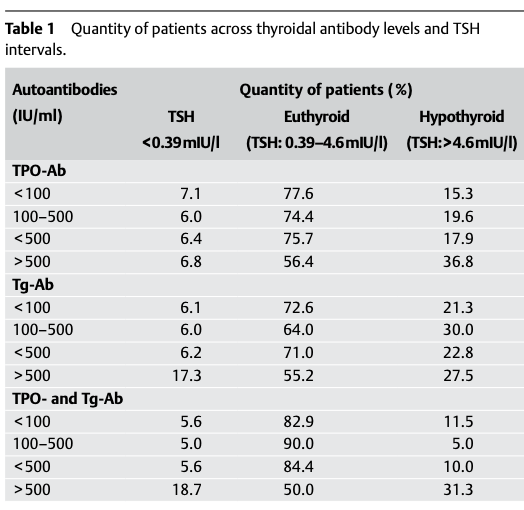
Is thyroid disease worse in those with higher antibody levels? A study tracked 335 people with thyroid disease for nine years to find out the answer. Specifically, it watched to see how their thyroid function slowed over the years and compared that to their antibody levels3. It turned out that antibody levels below 500 IU/mL stayed pretty stable. Those well over 500 IU/mL had more disease progression. This was true for either anti-TPO or anti-Tg. The effects were more dramatic when both were the same. If both were below 100 there was the least disease progression. If both were over 500, there was the most. When one or the other was high, the risks were pretty equal. In other words, high levels of anti-TPO was not worse than high anti-Tg. The following tables show how TPO-Ab compared to TSH levels in the study: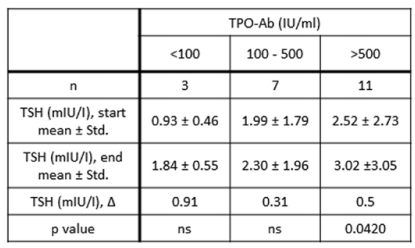
Symptoms
The symptoms from thyroid disease can be complicated. Many can arise from too little thyroid hormone and get better with thyroid medication. Others can come from related conditions like anemia or celiac disease. If you have taken care of everything else but still don’t feel well, thyroid antibodies can be the culprit. One study compared the symptoms of two groups of people who were on thyroid medication. Both groups had healthy thyroid levels, but one had higher antibody levels than the other. Those with the high antibodies had higher rates of several troublesome symptoms including changes to hair and voice as well as fluid retention4.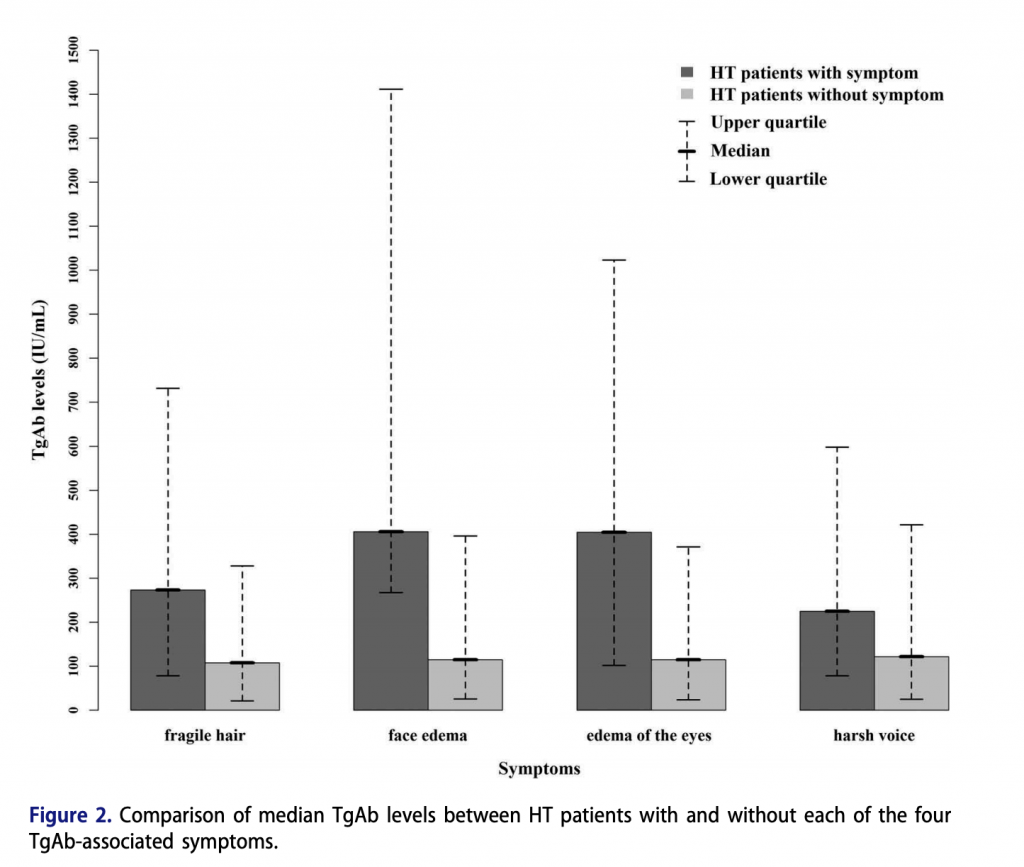
Cardiovascular Disease Risk
Thyroid disease relates to heart disease. It is well established that abnormal levels of thyroid hormones, in either direction, can be harmful to the heart and circulatory system. A recent study looked to see if antithyroid peroxidase antibodies related to cardiovascular risk in those with normal thyroid function. The results showed that: “TPO-Ab range was found to be significantly positively associated with atherosclerosis in eu-thyroid participants and in those participants with normal TSH range6”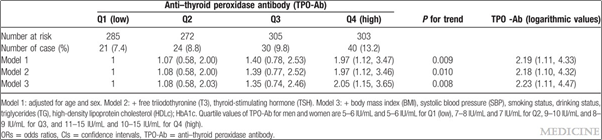
Fertility
Can thyroid antibodies keep you from getting pregnant? This one is not so straightforward. It is pretty clear that low thyroid function can worsen fertility. In most cases, people who are diagnosed with having thyroid antibodies also have low thyroid function. Specifically, low thyroid function seems to become a problem when TSH levels become higher than 4.0 IU/mL.- Soups
- Stews
- Stir Frys
- Smoothies (maybe not too much)
Is It Important To Lower Thyroid Antibodies?
Here is a quick recap of where we stand:
- Yes, for fertility or certain unresolved symptoms (like hair loss, swelling, or chronic fatigue).
- Yes, to prevent disease progression (if they are over 500 IU/ml).
- No, if thyroid levels are not yet regulated through diet or nutrition.
- No, if symptoms might be caused by other factors.
The Most Likely To Lower Thyroid Antibodies
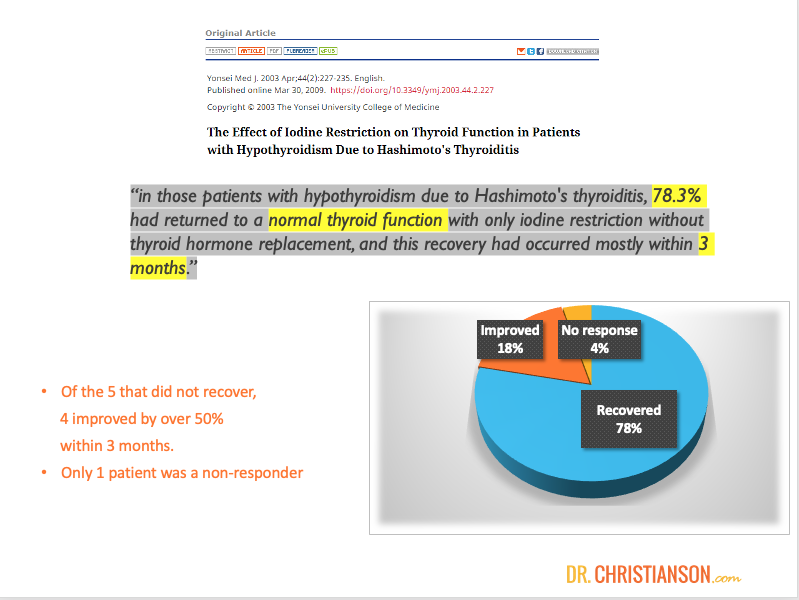
What is most likely to lower thyroid antibodies by a significant degree? Reduction in iodine to under 100 mcg per day, weight loss for those who need it, and supplements including selenium, inositol, and nigella. Let’s break each of these down in detail…1. Iodine Regulation
Iodine reduction is the first topic because it is the only intervention that has ever been shown to reverse thyroid disease. Other things may lower antibodies or help symptoms, and these are important outcomes. But, nothing else has ever been shown to cure people of thyroid disease. We’re going to cover iodine first, because it has the best evidence. And, because we hope that changing them will change the disease. In addition to that, because other interventions are unlikely to work if you aren’t watching your iodine carefully.How Does Iodine Regulation Help?
Earlier in this article, I mentioned how iodine drives autoantibodies to attack thyroid peroxidase and thyroglobulin. This fact has been known for some time. More recently, we even learned that iodine reduction may reverse thyroid autoimmunity. In the past, it was thought that thyroid autoimmunity would continue long term once it began. Now, we know that it often stops if the excess iodine can be eliminated.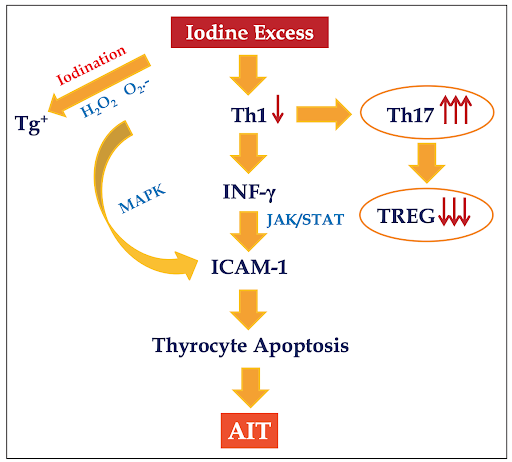
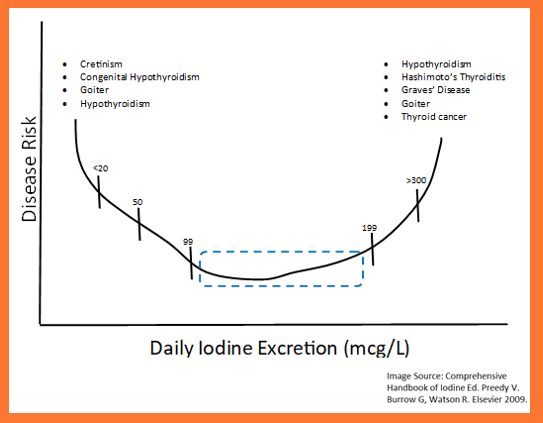
How Do You Reduce Excess Iodine?
The Thyroid Reset Diet explains the hidden sources of iodine and divides food by its iodine content into ‘green light,’ ‘yellow light,’ and ‘red light’ foods. The hidden sources that are not food include cosmetics, supplements, and medications. To clear the thyroid of excess iodine, one must simply avoid hidden sources of iodine and eat only green-light foods. This is pretty easy, because most all of the high-iodine foods have good substitutions that are low in iodine. When it comes to recommendations, The Thyroid Reset Diet gives comprehensive guidance on this process (as well as a bunch of really good recipes). I would be happy for you to check it out today!2. Weight Loss
We are so used to thinking about thyroid disease causing weight gain, but what if it went both ways? Most people understand the harmful effects of inflammation on the body. Many take turmeric supplements and eat blueberries in hopes of lowering inflammation. But, it turns out that fat cells can be the largest source of inflammation in the body13. As an example, it used to be thought that heavier people had more arthritis because the weight put more strain on their joints. We now know that weight is not the main factor. Joint pain comes on because body fat raises their inflammation levels14.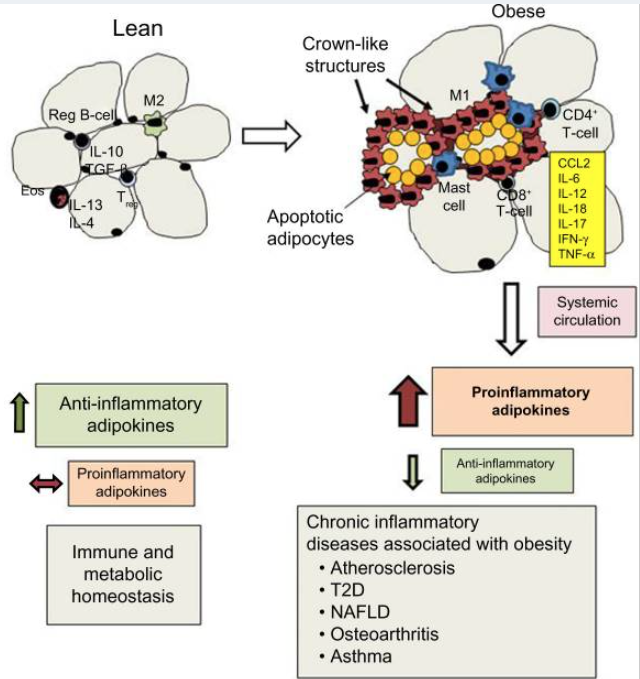
How Can You Lose Weight?
If weight loss has been difficult for you, first be sure that your TSH scores are not holding you back. To find which levels are best for you, visit the Thyroid Levels Calculator. Please note that TSH can be a problem both when it is too low and when it is too high. For those on thyroid medication, a TSH that is too low means they are taking too much. One that is too high means they are taking too little. Once your TSH levels are stable, follow the Reset guidelines in the Metabolism Reset Diet book. If you don’t have the book, you can also find many of its suggestions for free (Click Here: The Metabolism Reset Challenge). The basic idea here, though, is that you take 28 days and focus on weight loss. The main points of the program include:- Getting enough protein
- Limiting fats and carbs
- Exercising (but not too much)
- Eating foods to help your liver
3. Supplements
Countless supplements are purported to help thyroid antibodies. Yet, at the time of this writing, only three have been shown in human studies to lower thyroid antibodies. These include:- Selenium
- Inositol
- Nigella
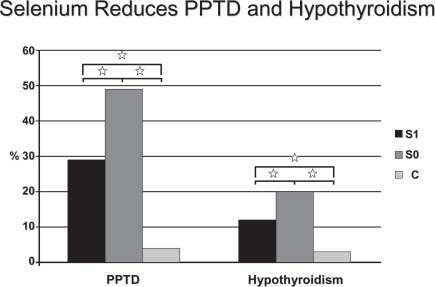
Selenium
Selenium is a lot of fun to learn more (Read More: My full guide to selenium and your health). In short, though, selenium helps the thyroid make glutathione. This is the antioxidant that protects the thyroid against oxidative damage from too much iodine. Thyroid antibodies elevate when this damage can no longer be controlled17.How Do We Know It Works?
It turns out that selenium in the diet and selenium in supplements may both be helpful for the thyroid. In The Thyroid Reset Diet, I encourage the ingestion of 2-4 Brazil nuts on a daily basis. Brazil nuts are one of the highest known food sources of selenium. Including them as part of a healthy diet can dramatically lower the risk of selenium deficiency. Several human studies have tested to see if selenium supplements can lower thyroid antibodies:- In one study in Germany, the use of selenium supplements for 3 months significantly lowered TPO-Ab, and improved the appearance of thyroid tissue on ultrasound18.
- In another study, people were assigned to take selenium or a placebo. Midway through, the groups switched, unbeknownst to the participants. Those taking selenium saw their TPO-Ab fall significantly, yet they increased while on the placebo19. Another study in Greece saw identical findings within 3 months.
- A French study of over 1800 participants found that selenium supplementation reduced the harmful effects of autoimmunity on the participants’ thyroid glands20.
How Should You Use Selenium?
Selenium should be taken in supplement form in addition to dietary selenium. I recommend an additional 50 mcg of selenium per day along with the amounts found in a multivitamin. Selenium is best taken with food and can be taken at the same time as other supplements. It is safe to take as soon as one hour after taking thyroid medications.4. Inositol
Inositol is a compound that acts like a b-vitamin.it has been known as Vitamin B825. Inositol is considered ‘conditionally essential.’ This means that some people are not able to make it internally and need to rely on their diets to obtain it. Foods with inositol include:- Fruit
- Beans
- Grains
- Nuts
How Does It Lower Thyroid Antibodies?
Inositol isomers are essential for communication between the brain and the thyroid gland. Some parts of this communication depend directly on the presence of inositol.How Do We Know It Works?
In a study of 48 people with Hashimoto’s disease, a supplement containing inositol and selenium was tested to see if it could improve thyroid function. They were tracked for a period of six months and compared against a group that received a placebo. Over the course of study, those taking inositol and selenium saw marked improvement. Their TSH levels lowered by 31% and their thyroid antibodies improved. TPO-Ab reduced by 42% and Tg-Ab came down by 42%. Roughly half saw their Tg-Ab levels go into remission. The participants also saw improvements on their ultrasound findings. None of these benefits showed up in the control group and no significant side effects were noted26.How Should It Be Used?
Inositol should be taken in supplement form in addition to dietary inositol. I recommend an additional 500 mg of inositol per day. Inositol is best taken with food and can be taken at the same time as other supplements. It is safe to take as soon as 1 hour after taking thyroid medications. Inositol within the dosage range I advise, has been shown to be safe in pregnancy. In fact, it seems to lower the risk of gestational diabetes27.5. Nigella
I have also written before about nigella sativa (Read More: All about nigella). It is a seed that has been used for thousands of years as a food and a source of medicinal oil. It is also called black cumin, black caraway, and kalonji. Historically it was used to treat conditions that relate to inflammation. Over the years stories emerged about its ability to help nearly any condition including:- Allergies
- Arthritis
- Asthma
- Autoimmune disease
- Cancer
- Diabetes
- Hair Loss
- High Cholesterol
- Hypertension
How Does It Lower Thyroid Antibodies?
We know that some compounds that act as anti-inflammatories may lower thyroid antibodies. Nigella has anti-inflammatory properties.How Do We Know It Works?
Multiple human placebo controlled studies have shown that nigella can help people with thyroid disease. In the first study, 100 people were recruited to receive nigella or a placebo for 8 weeks. During that time, the only intervention was the use of nigella extract. By the end of the eight weeks, those given nigella saw their thyroid function improve and their thyroid antibodies lower by an average of 50%29.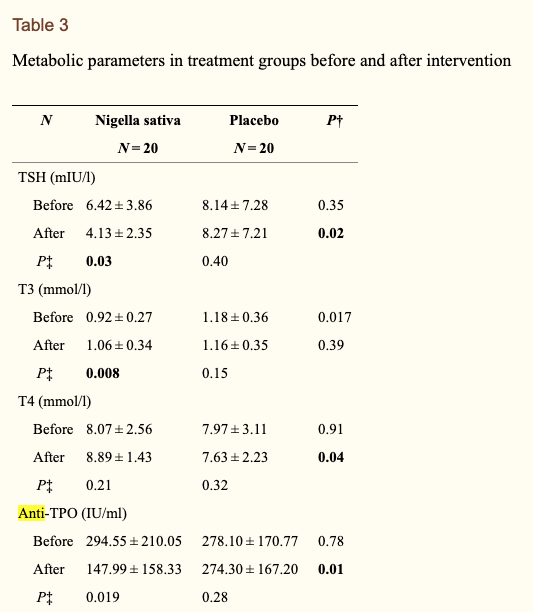
How Should It Be Used?
Nigella should be taken once daily at a dosage of 100 mg. It can be taken with or without food. It can be taken at the same time as other supplements. It is safe to take as soon as one hour after taking thyroid medications. Nigella is also safe in pregnancy when used at the advised dosage32.What May Help Lower Thyroid Antibodies?
The following items may be helpful but they differ from those that are most helpful. Some may help, but certainly do not apply to everyone. Others help, but only by smaller degrees. Others in this category have evidence suggesting they might help, but there are no human trials proving that they do. Let’s get into them…1. Vitamin D
Those prone to thyroid disease are more apt to be deficient in vitamin D than those who are not. This finding is plausible because vitamin D plays roles in inhibiting inflammatory interleukins and regulating the immune response33. One study did show that vitamin D supplementation may lower TPO-Ab in those who were vitamin D deficient, but the connection was weak34. The thing is, though, that we lack clinical trials showing that vitamin D supplementation clearly improves thyroid function or lowers thyroid antibodies in those with thyroid disease. A common trend in studies on vitamin D is for correlation to show up between a condition and low vitamin D. Yet, when follow-up studies are done to see if supplementing with vitamin D helps the condition, they usually do not.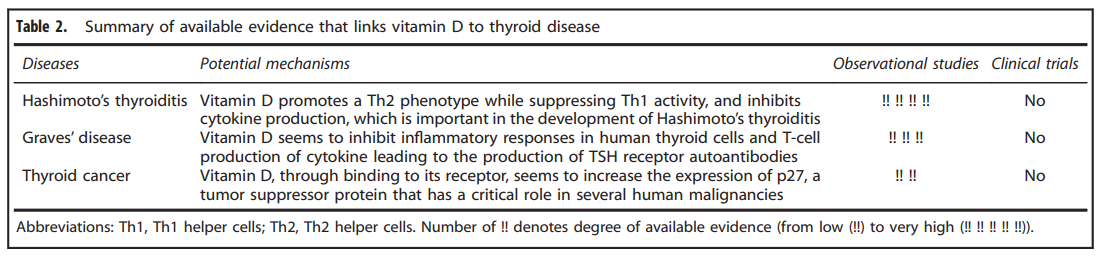
2. Sleep Apnea
Is your sleep unrefreshing? Have you been told that you snore or hold your breath at night? If so you may have sleep apnea. If you do, it may be part of why your immune system is attacking your thyroid36. There are some thoughts that apnea and thyroid disease may have a bidirectional relationship. Apnea may lead to the immune changes that cause thyroid disease and thyroid disease may lead to the weight gain that worsens apnea. Not everyone with thyroid disease has sleep apnea, but those who do may not improve until their apnea is managed (Read More: My comprehensive guide to sleep apnea).3. Thyroid Medication(If You Need It)
If you are already taking thyroid medication, don’t think that stopping it will lower your antibodies. If you are not yet on thyroid medication, but are considering it, you may have the option of doing The Thyroid Reset Diet first – please check with your doctor. It is commonly held that if your thyroid antibodies are high, your thyroid will quit working, but if they become negative, your thyroid can get better. Some worry that taking thyroid medicine will make their antibodies worse. They try to get off from their medication in hopes of helping their thyroid heal. It is true that if you take too much medication, your thyroid will be more apt to quit working. Yet, if you take too little, the extra strain on your thyroid can hurt it just as much. Studies have shown that when thyroid medication is given at appropriate doses, thyroid antibodies get better37.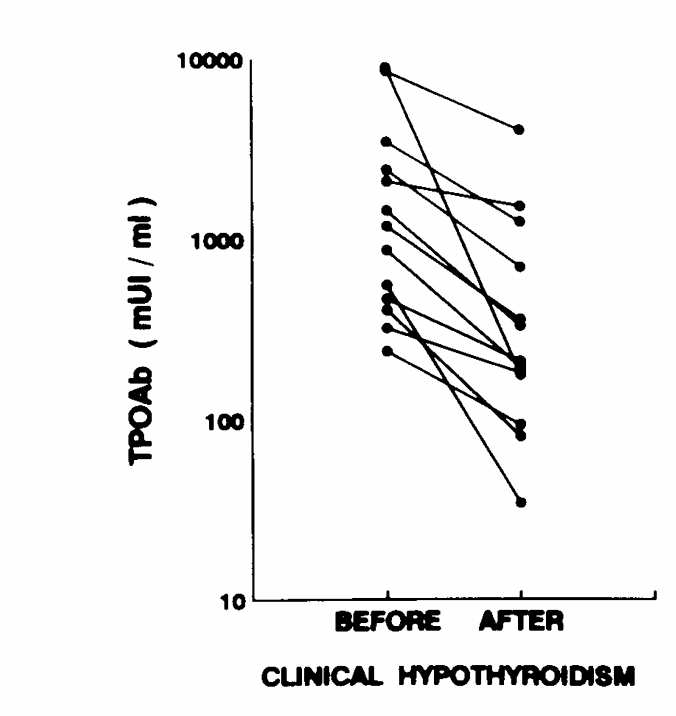
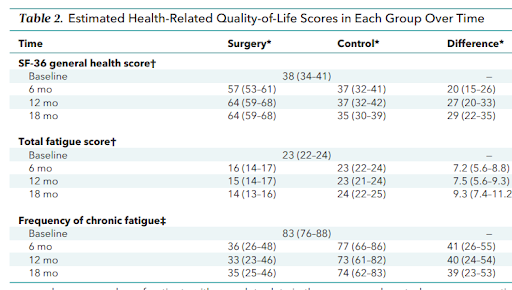
4. Natural Desiccated Thyroid
What about natural desiccated thyroid? Some say it can raise thyroid antibodies. The truth is the opposite, it typically has no effect, or it lowers them. There is a popular belief that natural desiccated thyroid like Naturethroid or Armour, is not safe for those with Hashimoto’s. Some thought that it would even raise antibody levels. Thyroid antibody levels can fluctuate for many reasons. I have no doubt that some people have seen their thyroid antibodies go up after they started taking desiccated thyroid. The real question is: Do more people have their thyroid antibodies go up after taking desiccated thyroid than you would expect by chance? The answer to this question is no. In fact, there is some evidence (albeit old) that taking desiccated thyroid may lower autoimmunity38. The theory is called oral tolerance and it is the same logic behind allergy treatments. With thyroid disease, the immune system attacks thyroid tissue. If you ingest a little thyroid tissue regularly, your immune system may become more tolerant of it. A study in 1998 looked to see how synthetic and natural thyroid compared in regards to immune responses. The findings were that natural thyroid lowered signs of autoimmunity without producing adverse changes in antibodies39. Many people who take synthetic thyroid and do not feel their best do better when they change to desiccated thyroid. In one study, people were given either natural or synthetic thyroid medication for 6 months. Halfway through, they were changed to the other and no one was ever told which they were taking. When asked which they preferred, roughly three times as many people felt better on desiccated thyroid40. If you are on synthetic thyroid medication and are struggling with your antibodies, changing to natural thyroid might help (Read More: You can find out more in my guide to thyroid medication).5. Food Categories
Besides iodine, what else do we know about diet and thyroid antibodies? You’d be amazed how little published data there is! I’ll mention gluten and AIP diets in the next section. The only other study that showed helpful results was one that looked at how the intake of various food categories related to thyroid antibodies. The study itself looked at 924 Croatians, roughly half of whom had thyroid disease. The intake of various food categories was compared between the groups.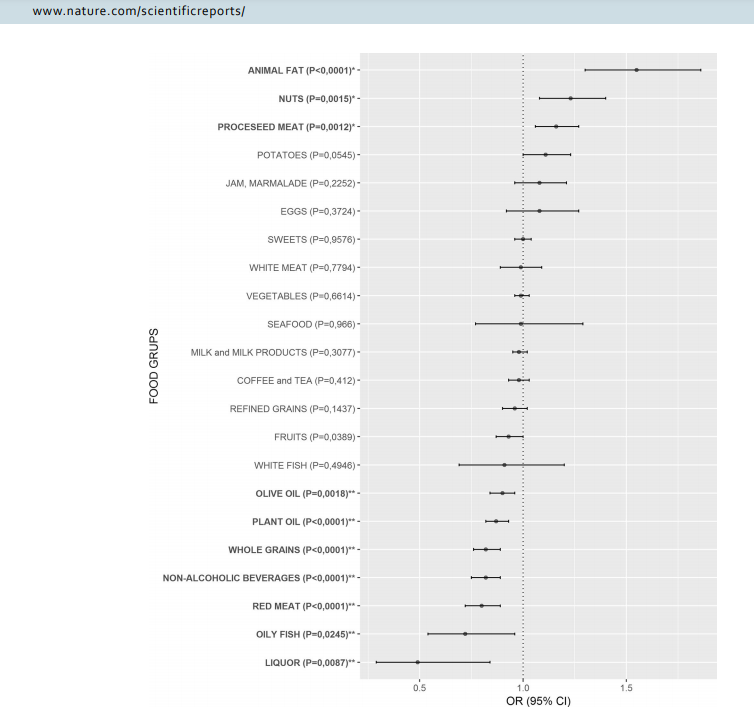
Not Likely To Help Lower Thyroid Antibodies
This last category includes popular items that have been talked about as ways to lower thyroid antibodies, but the evidence for them is pretty weak. You only need to read this if you were already curious about one of these options…1. NAC
NAC (n-acetyl cysteine) is an amino acid supplement that may help the body produce glutathione. One test tube study suggested that it may prevent the immune system from damaging thyroid cells. No animal or human studies have verified these findings42.2. Low Level Laser Therapy
Expert friends of mine were excited that this would be the answer to thyroid disease. Some even bought the lasers, but they never found them to be helpful. Several studies suggest that they may help, but they are all from the same researcher and the results are miniscule at best43.3. Gluten-Free Diets
Many go gluten free and feel better. Others need to go gluten free due to celiac disease. If either of those apply to you, please remain gluten free. People often tell me that they feel fine if they eat gluten, but they wonder if they need to avoid it because of their thyroid. The short answer is no. People with one autoimmune disease have a greater risk of having others. For this reason, many with thyroid disease have celiac disease. Some speculated that one causes the other or that gluten causes people with celiac to get thyroid disease. Yet studies on those with celiac have shown that just as many get thyroid disease whether or not they avoid gluten. In the study, a group of 128 people newly diagnosed with celiac disease had their thyroid function monitored for one year. Most (91) had normal thyroid function44. Of those who did not, 20 were hypothyroid of which six had positive Hashimoto’s antibodies. 1 was hyperthyroid and went on to be treated with medications. Some surprising results were:- A larger number of people with celiac and no thyroid disease (5) developed thyroid disease after going gluten free. It would not be reasonable to conclude that the gluten free diet worsened their rate of developing thyroid disease, it likely would have happened either way.
- Of the remainder of the 16 with normal thyroid function and positive antibodies, nine did not improve and four developed abnormal thyroid function.
- Within this year of those with other thyroid diagnosis, many got worse, a few stayed the same, and a few got better. Yet there were no clear differences between those who were compliant with the diet and those who were not.
4. Autoimmune Paleo Diet
If you have done the autoimmune paleo diet and found it helpful, that is fine. Hopefully the benefits will last for you, because the diet itself is far too restrictive to be followed long term. A study was done in which women with Hashimoto’s disease followed the autoimmune paleo diet for 10 weeks46. At the end of the 10 weeks, there were no apparent changes to their thyroid function.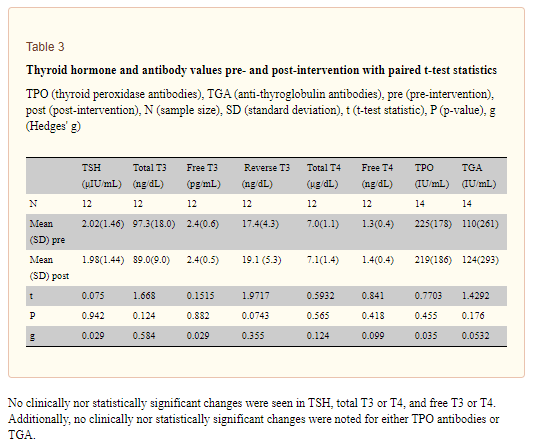
5. Low Dose Naltrexone (LDN)
LDN is purported to reverse thyroid autoimmunity and cause people to no longer need thyroid medications. Despite the considerable enthusiasm, there has only been one published study to date and it showed no effects47. If anything, those on LDN got worse. In it, 898 patients were tracked over a period of 4 years. The participants were on thyroid medications of various types + LDN at several different dosages. The researchers concluded that : “We found no association between starting LDN and changes in the dispensing of thyroid hormones. If anything, there was a tendency towards increasing LT4 consumption with increasing LDN exposure.” I have heard from countless people who have tried it. Some felt fatigue as a side effect, but none told me that it improved their thyroid function or even lowered their antibodies. This is another example where people think it would work because of mechanisms, but it does not work in practice.6. GI
If you do a google search about how to lower thyroid antibodies, the most common responses involve treating leaky gut or dysbiosis. Gut health is essential to overall health. There are ideas by which changes in gut health may increase the odds of developing autoimmune diseases. It is for these reasons that many popular blogs claim that treating dysbiosis or leaky gut is essential to lowering thyroid antibodies. There are strong ties to thyroid disease and gut health…. People with thyroid disease have a 2-5 fold higher risk of having celiac disease48. Organisms like blastocystis hominis and helicobacter pylori are more common in those with thyroid disease as is small intestinal bacterial overgrowth. As many as 40% of those with thyroid disease may have an additional autoimmune disease that harms their stomachs. This condition is called atrophic gastritis and can lead to poor nutrient absorption and risk for intestinal cancers49. If one has any intestinal issues, it is important to find the reason behind them and do as much as possible to resolve it. But will doing intestinal tests or treatments help lower thyroid antibodies? The only study to date that addressed this question was one in which those with thyroid disease were treated with a probiotic. The participants were on thyroid medication, and most of them had positive thyroid antibodies50. Why is there such a disconnect between the research and the buzz? The idea that leaky gut raises thyroid antibodies comes from the idea that gut permeability causes autoimmune diseases. It was an idea that was seriously considered in the early 2000’s. One of the largest pitfalls in medicine is the allure of disease mechanisms. It seems that if we know how a disease starts, we automatically know how to fix it. If autoimmune disease is caused by leaky gut, then treatments that help leaky gut must help autoimmune disease. The problem is that our model of how diseases work are not always right and even when they are, fixing the cause does not always resolve the problem. You can never assume a treatment works because it makes sense with our current understanding. You can only say that it works when you have seen it work. We don’t have studies showing that leaky gut treatments lower thyroid antibodies or treat thyroid disease. Our understanding of leaky gut has evolved greatly in the last decade even though the popular ideas about it have not. It is true that many people with autoimmune disease have more permeable (leaky) intestinal linings than others. But did this cause their disease, or is this because of their disease? If it caused the disease, you would expect that treating leaky gut would reverse the disease. You would also expect that if you treated the disease in some other way, leaky gut would remain. Neither of these have born out. GI Treatments Summary:- If you have digestive issues, it is worth getting a proper diagnosis to help guide you to effective treatment and to detect any risks.
- Treatments for leaky gut, dysbiosis, or other digestive issues have not been shown to improve thyroid function or lower thyroid antibodies. The single study to date showed that probiotics do not lower thyroid antibodies.
Lowering Your Thyroid Antibodies Today
I hope this guide gave you a helpful rundown of the things that we know help lower thyroid antibodies, where the evidence is interesting but not strong, and where the evidence simply is not there at all. In short, when it comes to your thyroid, knowing more about it is so important. That’s why I would love for you to take the Thyroid Quiz today (Click Here: Take The Quiz), to gain a bit more insight into your thyroid and where it currently stands.Resources