I always appreciate whenever someone writes in to ask me a question about their health. I recently received a message from Remy about depression, and I wanted to do a deep dive on the subject to help clear up any confusion – and address some action steps.
Here’s what Remy wrote:
“Hi Dr. C,
Something has been wrong and I’m not sure what to do. I just don’t find myself happy anymore. I never seem to be able to get enough sleep and I’m always down on myself.
I have no reason to be upset because I have a lot of things I should be thankful for. My guess is that I’m depressed. I don’t believe in taking pills for it. I already take pretty good care of myself. I googled natural remedies but I’m not sure what to believe.
You explain things really well and I trust you. Do you have any articles about depression or any advice?” – Remy
Understanding Depression
Hi Remy,
I’m glad you had the courage to reach out and the clarity to see that something was amiss in your life.
Many people in your situation take their feelings at face value and let them cloud their perception of their situation and see it as the culprit.
Many also lack the ability to see that they are in a state that can pass, they mistake feelings for parts of their core identity.
You already have the first two ingredients that are essential for recovery, so kudos to you.
You’re right. These are feelings that are often categorized as depression. More often then not, labels can carry their own stigma but they can also be a useful way to predict the best strategies.
Your note really struck a chord with me. I have also dealt with this, firsthand, as well as with many family members and patients.
Key Insight: There may be some underlying medical issues and these are all important to touch upon. But, what I want you to hear is that you can feel better.
It can take some time and you might have to pivot once or twice but you can feel better.
I’m going to pull together what I’ve learned, what I’ve experienced, and the latest research to give you a proper answer.
Depression: Summarized
The annotated version is that I see depression as a combination of four factors:
- Health
- Habits
- Life
- Thoughts
There is usually a combination of factors at hand for any given person, but some can have more bearing on some people than others.
The solution is to think through all of them and address those of which may be relevant for you.
Pull up a seat and let’s talk it through.
Understanding The Terms
Emotional depression is a feeling of severe despondency and dejection.
Clinically, depression is a collection of symptoms, such as the above, that are lasting for over two weeks and have no discernible physical cause.
Depression commonly overlaps with anxiety. There are also many variants and subtypes of depression including:
- Major
- Atypical
- Situational
- Dysthymia
- Manic
Which type is most likely for you? Such distinctions are not always essential to your progress. If needed, they need the help of a certified professional.
What are the Symptoms of Depression?
What comes with depression is its own set of symptoms that are critical to recognize.
Here’s what you need to know:
Mood Symptoms
Mood symptoms can include:
- Fear for no clear reason
- Lack of pleasure from normally enjoyable activities
- Unexplained sense of guilt
- A higher or lower appetite than normal
- Fatigue
- Poor sleep or unrefreshing sleep
- Issues with concentration
- General sadness
- Edginess
- Irritability
- Avoidance of company
Physical Symptoms
Along with some of the classical mood symptoms. For many, these will be entirely unexpected.
Some of the top unexpected symptoms include:1
- Lower back pain
- Irritable bowel syndrome
- Migraine headaches
- Fibromyalgia
- Burning hands and feet
- Fatigue
It gets tricky. These symptoms can be caused by many things besides depression. Yet they also respond well to therapy that only addresses the mind.
Dr. John Sarno’s work with lower back pain is a strong example. His treatment for low back pain involves explaining how stress and tension can cause it. As well as how mental strategies can help reverse it.
Clinical trials have shown that his approach can be more effective than typical interventions for back pain especially in populations with severe back pain lasting greater than 3 years.2
Depression can cause real changes in parts of the body outside of the brain. It can also cause the brain to have different responses to normal signals from the body.
Part of the common mental response with depression can be an increased focus on physical symptoms and a persistent sense of needing to find answers and explain things.
Bottom Line: Put all of these patterns together and you could see how it would be difficult to accept that depression can be the prime cause of physical symptoms. This dismissive attitude expressed by some in the medical community only makes things worse.
How Common is Depression?
One thing is for certain: you are not alone.
This is extremely common, and that fact alone can be a source of relief.
The sense of isolation from thinking that no one else has been through this perpetuates depression by itself. Please let go of that right now.
Because many do not get a proper diagnosis and care, the numbers are murky. Credible estimates suggest that in a given year, 30% of adults will have a diagnosable mood disorder like depression.
In any specific week, 10% of adults will be clinically depressed. Up to 25% of all people will experience major depression at some point.3
Some even argue that it is the most common medical condition worldwide.4
It may be getting more common in younger generations. According to one survey, a full 90% of those in Generation Z (ages 15-21) have experienced significant depression.
Bottom Line: We are not sure just yet how much this represents a higher stress load and how much this represents a greater willingness to talk about mood symptoms.5
What Triggers Depression?
For many, depression comes on after major life events like the loss of a loved one, changes at work, suffering from abuse, or moving to a new area.
Please consider that even what we might consider as “positive” changes can trigger depression if they significantly alter your routine.
If depression comes on after an incident like these, it is still real and still warrants treatment if it is affecting the rest of your life.
It may get better on its own, but there are no awards to be won by soldiering through adversity longer than needed.
Genetics of Depression
The most common perspective is that depression is an interplay between genetics and environmental factors:
“The influence of genetic factors is around 30-40%. Non-genetic (environmental) factors, explaining the remaining 60-70%.”6
Despite the apparent wisdom, on gentle inquiry, that statement becomes vacuous.
Besides genetics and environmental factors, what else could affect any facet of our health? Seriously, think about it. Every variable we know of goes in one of those two buckets.
When you distill it down, it is no different than saying – we know that certain factors cause depression.
Even if there were an evil clown that randomly chose who would be depressed, that would still be an environmental factor.
Key Insight: The question that matters is whether anyone is stuck with depression because of their genes? The short answer is no. The link is much less strong between genes and depression than it is for genes and bipolar disorder or schizophrenia.
Depression is more common among those with a family history of it, but most people with a family history of depression do not suffer from depression.
There are many gene variations more common among people with depression, but none are close to direct causes.
All the relevant genes are influenced by countless other genes and other situational factors in ways that leave them with zero predictive value.
In short “there is no solid evidence for specific genes and specific gene-by-environment interactions (as the causes of depression)”7
Specific Genes: MAOA Gene
One gene with large amounts of research connecting it to depression is called the MAOA gene or the warrior gene.
Some pop-health info has led people to believe that if they have this gene variant they are more at risk for mood issues and they need to take certain supplements to prevent them.
One of the top genetic researchers addressed this phenomenon directly and argued that, by their estimation, any self-fulfilling effect brought about by thinking this was true would be immeasurably larger than the effects from the gene itself.
Key Insight: In other words, thinking your genes will cause depression will affect you more than having genes that cause depression.
In the case of your mood, genes are not destiny. I have written about this in the past and would love for you to take a look now to learn more (Click Here).
ACE Scores
If genes don’t predict depression, what does? Early life trauma is likely the single strongest predictor.
ACE stands for Adverse Childhood Experiences. One’s ACE score is a composite of how many significant negative events occurred before age 18 (out of 10 possible events).
The events include things such as:
- Physical abuse
- Neglect
- Sexual abuse
- Incarceration of a family member
- Separation/divorce of parents.
The negative side of focusing on early-life trauma is that it can elicit a sense of helplessness. For each person who succumbed to trauma, there are just as many more who were inspired to create a new path because of it.
Bottom Line: ACE scores fail to take into account the variabilities of individual resilience and the potential to find strength after trauma.8
Health
The human brain is only about 3% of our body weight, but it uses up about 25% of our energy.
In order to work at its best, it needs a more exacting balance of fuel, building blocks, and micronutrients than any other part of the body.
Key Insight: Any part of your health that is not optimal can compromise your brain’s performance and predispose you to depression.
Nevertheless, some health conditions are more insidious than others and are more common in the populations prone to depression.
Some of the typically undiagnosed physical issues that can cause depression or worsen its symptoms include:
- Thyroid disease
- Parathyroid disease
- Autoimmunity
- Diabetes and pre-diabetes
- Anemias
- Nutrient deficiencies – B12, folate, zinc, vitamin D
- Kidney disease
- Seasonal affective disorder
- Sleep apnea
- Heart disease
- Adrenal stress / HPA abnormality
- Arthritis
- Obesity (which may also cause depression)9
In resolving depression, you’d want to do a good physical exam and comprehensive blood tests with a special eye on the above conditions.
At what point do you quit searching for physical causes and focus on treating depression? Furthermore, what if a possible physical cause has been identified, you’ve started treating it, but you still feel depressed?
I have often heard doctors talk about doing things in certain orders. Treat this first, then that.
I understand how this could be helpful for writing up a nice study, but when a person is suffering, why wait?
The best first steps to treat depression are good ideas onto themselves. The only risk is that you might develop more healthy habits and insights on the human condition than you absolutely needed – I’m not too worried about that.
Thyroid and Depression
If you’re following my work, there is a good chance that you do so because you have had an issue with your thyroid. The link between undiagnosed or inadequately treated thyroid disease and depression is really very strong.
In a recent study, 93 patients with Hashimoto’s Thyroiditis and normal TSH levels were checked for depression and compared to a similar group of people free of apparent thyroid disease.
Of those with thyroid disease, 49 had stable thyroid levels without medication and 44 were on T4 replacement therapy. Examples of T4 replacement include Synthroid, Tirosint, and levothyroxine. The thyroid blood levels were similar in all groups – those with or without thyroid disease and those on or not on thyroid replacement.
Compared to those without thyroid disease, those with Hashimoto’s had nearly twice as high scores on the surveys for depression (5.0 vs 9.5).
For those with thyroid disease, the higher the TSH score within the normal range, the higher their rate of depression.10
Researchers in the psychiatric community have proposed a TSH cutoff of 2.5 for patients with depressive symptoms.11
What About Thyroid Antibodies?
There is also some evidence that positive antithyroid peroxidase antibodies (TPO) may be associated with symptoms even in those who have normal thyroid function.
In one such study, 47 patients with Hashimoto’s Thyroiditis with elevated TPO antibodies were compared against 17 patients with Hashimoto’s who had negative antibodies. All had similar levels of TSH, free T4, and free T3.
Those who had the highest levels of TPO for over three years had the highest risk of mood symptoms including depression and related symptoms of somatization (physical symptoms of depression.)
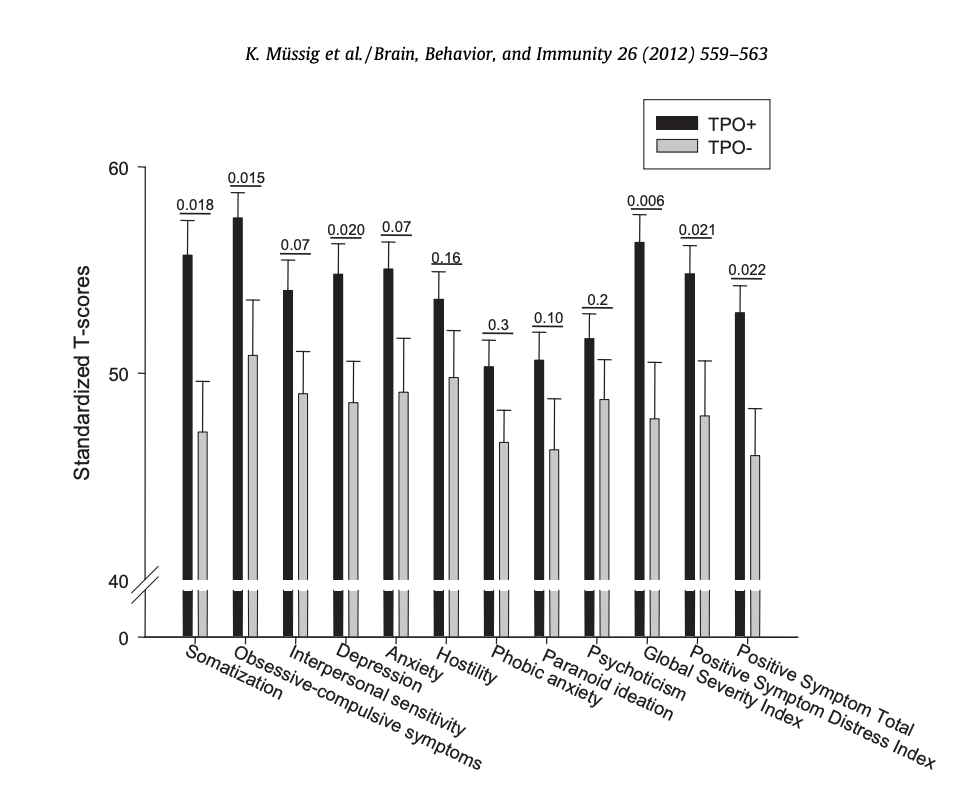
Note that minor antibody elevations did not as strongly predict depressive symptoms. The antibody levels that seemed to be relevant were those greater than 1586 IU/l.12
Key Insight: If you do have thyroid disease, you are more apt to have unresolved symptoms of depression when your TSH is on the high side of the optimal range (or if your TPO antibodies are well over 1000 IU/l).
With thyroid hormones, more is not better. A TSH reading below 0.35 is indicative of early hyperthyroidism. Many well-intended doctors over-medicate patients on thyroid treatment believing that if too little can cause depression, a little extra could help with it.
Bottom Line: Unfortunately, too much thyroid hormone can also be a driver of symptoms as common as depression but also as severe as psychosis.
In fact, there are case reports of patients with long-standing histories of mental illness and mild hyperthyroidism in which psychiatric medications have no effect until thyroid levels are normalized.13
Please know that if you are not getting answers, you can always connect with one of our doctors at Integrative Health to help get more clarity with your diagnosis (Click Here).
Depression and Thyroid Action Steps
If you have depression and have not been diagnosed with thyroid disease, look past the normal range.
A full thyroid workup should include tests for:
- TSH
- Free T3
- Free T4
- Thyroid antibodies
- Thyroid ultrasound
A healthy TSH is between 0.4 – 1.9. Learn a little bit more about why that matters with the following link (Click Here).
If you are on thyroid treatment, you should consider:
- Working to reduce your TPO antibodies (to below 1000)
- Optimize your TSH
- Considering natural desiccated thyroid over synthetic thyroid hormones
Medications as Causes of Depression
Depression can also be a medication side-effect. Some of the most commonly used culprits include:
- Blood pressure medications like atenolol
- Certain antibiotics, especially when used repeatedly, like ciprofloxacin14
- Oral contraceptives
- Agents like Lipitor
- Corticosteroids like prednisone
- Anxiety medications like Xanax
- Sleep aids like Ambien
These are not the only culprits. If your symptoms came on within a few months of starting a medication, consider it a possible culprit and talk to your prescriber.
Maybe your medication is no longer needed, or another with less risk for depression could be substituted.
Habits
Habits are so important for your health. Here are some that make a big difference:
Exercise
Exercise is great for prevention and is clearly helpful for treatment. While the consensus is that it helps, there is some debate as to how much it makes a difference.
Most of the available data revolves around aerobic activity, with no research on strength training, high-interval intensity training, or mixed activities and depression.
When it came to aerobic research, supervised activities were more effective when a group class or trainer was involved.
Key Insight: A 50 – 80% maximum heart rate is the ideal intensity, with 45 – 60 minutes, 5 times per week, seems ideal.15
Fish Oil
Fish oil has been studied as better than a placebo and has been known to reduce HRSD scores by 12.4 (versus 1.6 for placebo).
Overall, it may help due to:
- Anti-inflammatory Action
- Direct Membrane Modification
- Indirect Membrane Modification
Bottom Line: Fish oil has been studied as perhaps most effective for those with measurable chronic inflammation – and safe and studied in combination with other medications.16
Veganism
Most of the data on omega-3 fats and depression specifically look at EPA and DHA from fish oil. For those who wish to avoid fish products, you still have options at hand.
In the diet, many seeds and seed oils are rich sources of alpha-linolenic acid (ALA.) ALA is a substance that the body can turn into the main omega 3 fats eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA.) The conversion of ALA into DHA is often the trickiest step.
Those who are low in zinc or taurine may have a less active delta 5 desaturase enzyme. Those with higher total fat intakes can also have this same difficulty.
Key Insight: Vegans with healthy intakes of plant protein, adequate zinc, and lower fat diets generally do the best making EPA and DHA out of ALA from plants.
The other option is that EPA and DHA are now both synthesized from algae into supplements that many vegans do find acceptable.
Diet and Depression
Can foods help with depression?
In the most comprehensive evaluation of foods and depression, nutrients were identified that have been shown to lower the risk of depression based on 1628 individual studies.
These include:
- Folate
- Iron
- Long chain omega-3 fatty acids (EPA, DHA)
- Magnesium
- Potassium
- Selenium
- Thiamine
- Vitamin A, B6, B12 and C
- Zinc
These micronutrients are worth supplementing within the context of a good multivitamin.
If you do have thyroid disease, be sure you avoid all multivitamins that contain iodine. Potassium and iron are special cases.
Vitamins cannot have a full supply of potassium, because supplemental potassium is dangerous for certain populations.
Thankfully, it is found in all types of produce. Iron is important to take if you need it, but good to avoid if you do not.
Iron deficiency can be a recalcitrant cause of depression. Many who are low due to their menstrual cycles find that iron pills do not always raise their iron.
In these cases, intravenous iron can be a great option. For most, once a few IV doses bring up their iron supplies, it is easy to keep them stable from dietary or supplemental iron.
Key Insight: The best strategy to reverse depression is to eat a diet rich in these micronutrients and have a supplemental intake as a backup.
Food Rankings
In the next step, foods were ranked based on how much of those nutrients they provided per calories in a 100-gram serving. This ranking was called an antidepressant food score (AFS).
The food groups with the top rankings include:
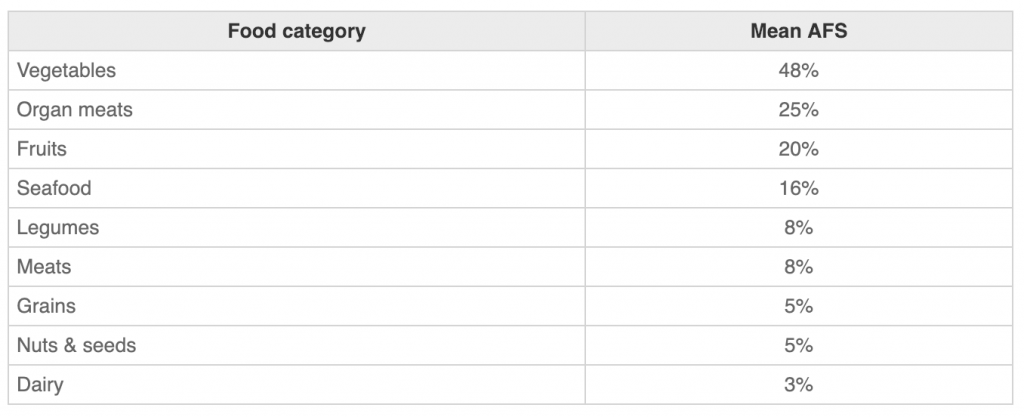
Individual foods were broken down into both animal and plant foods. Here are the top-scoring foods17:
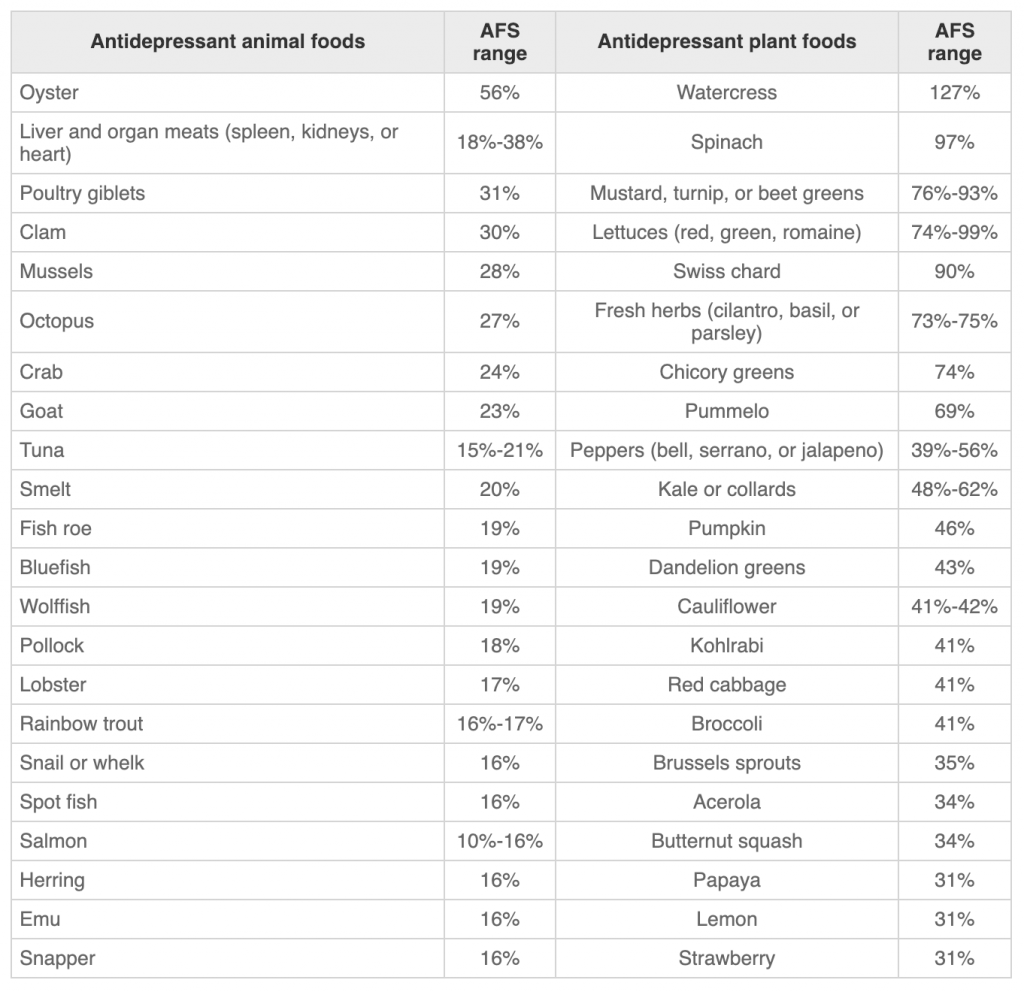
Studies have shown that some foods seem to raise the risk of depression and may make treatments for depression less effective. These include:
- Processed meat
- Refined grains
- Sweets
- High-fat dairy products
- Butter
- High-fat gravy18
Higher protein diets
Diets that are richer in high-quality protein have been shown to be helpful at alleviating depression, especially among people who are genetically more prone to depression.19
Good Carbs
Adequate amounts of protein and good carbs may also be important for managing depression. Glucose is necessary for the conversion of 5 hydroxyindoleacetic acids into melatonin.
Key Insight: Inadequate melatonin production can impair sleep quality and prevent the brain repair needed to heal from depression.
The way the reaction works is that there is a balance in the blood between tryptophan and large neutral amino acids (LNAA.)
Only when tryptophan (TRY) is higher relative to LNAA can 5 hydroxyindoleacetic acids cross the blood-brain barrier allowing for the production of serotonin and melatonin in the brain.
High-quality protein allows for available amounts of tryptophan.20
Good carbs in the diet lower the amount of LNAA in circulation improving the TRY/LNAA ratio. Protein foods alone cannot cause the production of melatonin because by themselves they raise the levels of LNAA even more than that of TRY.21
What about the Thanksgiving TRY theory? Well, it’s all a myth. Turkey is one of the lowest sources of TRY among animal protein sources. Post-Thanksgiving fatigue is simply from overeating.
Negative Habits
Beyond productive habits, there are those which need to be considered. Here are some potential negative habits, and how they affect depression, for you to keep an eye on:
Caffeine
A higher intake of caffeine can relate to higher scores of depression, anxiety, and insomnia. The same study also showed higher intake correlated to higher body weight and lower academic performance among students.22
Key Insight: Data is mixed, and some populations show different results.23 If you are depressed and you do use caffeine, test avoiding it for around 4 weeks.
It may or may not be a factor If you are depressed and you do not use caffeine, but there is no evidence to suggest that it will reverse your symptoms.
Alcohol
There is no debate that alcohol abuse can be a causative factor for depression.24 But what about the role of a glass or two of wine per day?
Studies like the PREDIMED study suggest that those with a low intake of wine have lower risks for depression than those who do not consume any.25
However, this study and others that show benefits to alcohol consumption fail to distinguish between categories of non-users.
Those who do not consume alcohol either do not by choice or do not for some medical reason – those who do not drink and those who cannot drink.
The most common reasons include former abuse of alcohol, impaired liver or kidney function, or chronic medications that cannot be safely combined with alcohol.
Key Insight: Those who can’t drink have higher rates of depression, cardiovascular mortality, and early death than those who do not.
Once you factor in the difference between those who don’t drink from those who cannot, the possible benefits to depression or longevity from low alcohol intake vanish.26
If you are depressed and you drink alcohol, even just a glass of wine per day, stopping it may be part of the solution. If you find the idea of stopping it to be difficult, think about what that means.
Bottom Line: Alcohol dependence can be one of the symptoms of depression. If you are depressed and you do not drink alcohol, there is no evidence that starting it will help you feel better.27
Can CBD Help Depression?
What about CBD oil? The short answer is that we do not know if it really helps, makes things worse, or does anything at all.
Despite a lack of large-scale clinical trials, people continue turning to CBD oil. But that has not stopped more and more of these products from entering the market.
Bottom Line: The long-term effects of CBD use remain unaddressed, specifically in certain populations. This means that we really cannot draw any concrete conclusions about these sorts of products.28
Life Changes
Studies done in the United Kingdom have shown that for a subset of people, a significant life change may completely cure depression.
In the study, some with depression were treated with medication, others spent time with an ‘ombudsman.’ This was really just someone who spent time with them and listened to their concerns.
A certain number of people found themselves inspired to make major life changes. Those who did were found to be free of depression with no other intervention even after long-term follow-up.29
Think about the large brush strokes in the painting of your life. Where do you live? What do you do? Who are you with? Are you making life better for those around you? Are you in alignment with your values?
Think about your connections with others. How many do you have? Are they close? Do you often spend time with them? There may be no single larger cause or solution than your connections.
If any of these are way out of sync for you, start here. Nothing else you do will likely help you feel better.
Bottom Line: These are questions we should never completely forget. Our lives are always a work in progress. Once you feel you have some momentum on the most important parts of yours, consider your lifestyle as well.

Recurrent Thoughts
Part of the cycle of depression is perpetuated by recurrent thoughts. An upsetting thought is experienced and we strive to fight or distract ourselves from it.
Often these strategies do not completely work or they have some negative consequences of their own which further drives depression. This, in turn, leads to more negative thoughts.
For most people with depression, part of recovery lies in developing a new relationship with one’s thoughts. It turns out that just deciding to think differently or reciting positive affirmations tend not to work.
Cognitive Behavioral Therapy (CBT)
CBT is a set of skills that help people see through counterproductive thoughts and more effectively solve immediate problems.
It provides systems that help a person analyze the content of their thoughts and determine which are reasonable and worth responding to and which are not rational and therefore are safe to ignore.30
Key Insight: When you are working with a practitioner, understand that you will get the best results when you find someone with whom you can establish a meaningful connection.
Cognitive Behavioral Therapy for Insomnia
This is a specific subtype for those with poor sleep. It works well because 90% of those with depression also have sleep issues.31
This is a strategy that may work with telehealth, but the studies are mixed overall but most studies show that it works as well (or almost as well).
ACT
Acceptance and Commitment Therapy is a newer version of CBT that has developed a strong body of evidence. It seems to be:
- As effective (or even more effective) for anxiety and depression32
- May help with issues concerning chronic pain33
- It may be especially helpful for chronic diseases when stress can be a component34
- Can be delivered one on one, in a group setting, or via online training
One facet of ACT is that it aims less at questioning the contents of thoughts and instead focuses on not being ‘fused’ to thoughts that are hurtful or unhelpful.
Bottom Line: Simple exercises are taught that help people identify unhelpful thoughts and quickly ‘defuse’ from them.
Mindfulness
We spend much of our lives deeply immersed in discursive thought. Whereas Cognitive Behavioural Therapy helps us identify inaccurate content of thoughts, Mindfulness helps us cultivate a state of awareness that exists apart from thought.
The goal and expectation are not to stop thinking or empty one’s mind, but rather to have glimmers of experience at a level of attention that precedes the spontaneous eruption of thought.
The more trained one becomes at reaching this state in structured practice, the more readily one can disentangle themselves from painful internal dialogues.
Mindfulness-Based Stress Reduction (MBSR)
This is an effective option that can treat current depression, and can also cut the risk of recurrence down the road. It may also work through:35,36
- Workbooks
- Apps
- Online protocols
- Other self-help formats
What About Antidepressant Medications?
Most psychiatrists or primary care physicians argue that antidepressant medications are the best place to start, and It is a compelling story.

Depression is caused by too little serotonin between the brain cell synapses. Sustained selective reuptake inhibiting (SSRI) medications cause the serotonin levels to go back to a pre-depressed state in effect healing the brain.
Numerous studies have shown that SSRI’s help about 50-70% of those with depression.
Of those who are not helped, another 50-70% are helped by switching to another medication or one that also works on norepinephrine called serotonin and norepinephrine reuptake inhibitors (SNRI’s.)
This is a helpful bit of text compliments of our friends at WebMD:
“If you’re being treated for depression, taking an antidepressant may be part of your treatment plan.
“Antidepressants work by balancing chemicals in your brain called neurotransmitters that affect mood and emotions. These depression medicines can help improve your mood, help you sleep better, and increase your appetite and concentration.
“Antidepressants can help jump-start mood and give people the boost they need to get over the symptoms of their depression,” says Eric Endlich, Ph.D., a clinical psychologist based in Boston.
“This often allows them to start doing the things they enjoy again and make better choices for themselves, which also helps contribute to a more positive mood.”37
Unfortunately, as simple and as tidy as this story is, none of it is true.
- Low serotonin does not cause depression
- SSRI medications are not more effective than placebos
Those are some strong statements. Let me back them up and explain why I do not consider SSRI or SNRI medications as first-line treatments for depression.
Failed Serotonin Hypothesis
The theory that low levels of neurotransmitters were the cause of depression first came from Joseph Schlidkraut in 1965.38 Serotonin became the molecule of focus within the next two years.39
Numerous attempts were made to prove the hypothesis. Researchers measured serotonin by-products in the cerebrospinal fluid in those with severe depression.
They also tried to cause depression by depleting serotonin. Other attempts were made to reverse depression by giving massive doses of L-tryptophan, a precursor of serotonin.
None of these efforts worked.40
Key Insight: More modern neuroscience has tried to find evidence of abnormal serotonin in those who are depressed and also found no support for the serotonin hypothesis.41
Where does the story come from and why is it so persistent? Scientists have identified marketing materials from SSRI manufacturers as the main source.
Their reasoning is circular: They start out assuming that depression is caused by low serotonin (it is not) and then assume that since their medications work, that they must raise serotonin.
Before we even talk about whether or not SSRI medications work for depression, the problem with this reasoning is that many things that are known to not affect serotonin can help improve depression.42
These same companies now claim that ‘low serotonin’ is the culprit behind numerous other conditions such as obsessive-compulsive disorder, premenstrual dysphoric disorder, fibromyalgia, and social anxiety.
The purpose of the claim is to justify the use of SSRI medications in these conditions despite the fact that none of these conditions have been proven to be caused by low serotonin.43
Mechanisms of Depression
The current consensus is that monoamine neurotransmitters such as serotonin, are not the cause of depression are represent the effects of other upstream changes in brain function.44
So, what are the mechanisms behind depression? Right now we do not have any solid answers.
We know that genetic factors, gender, early-life traumas, stress hormones, and inflammatory chemicals are part of the story, but no one factor pulls it all together.
The following table shows the current theories and their individual strengths and weaknesses:45
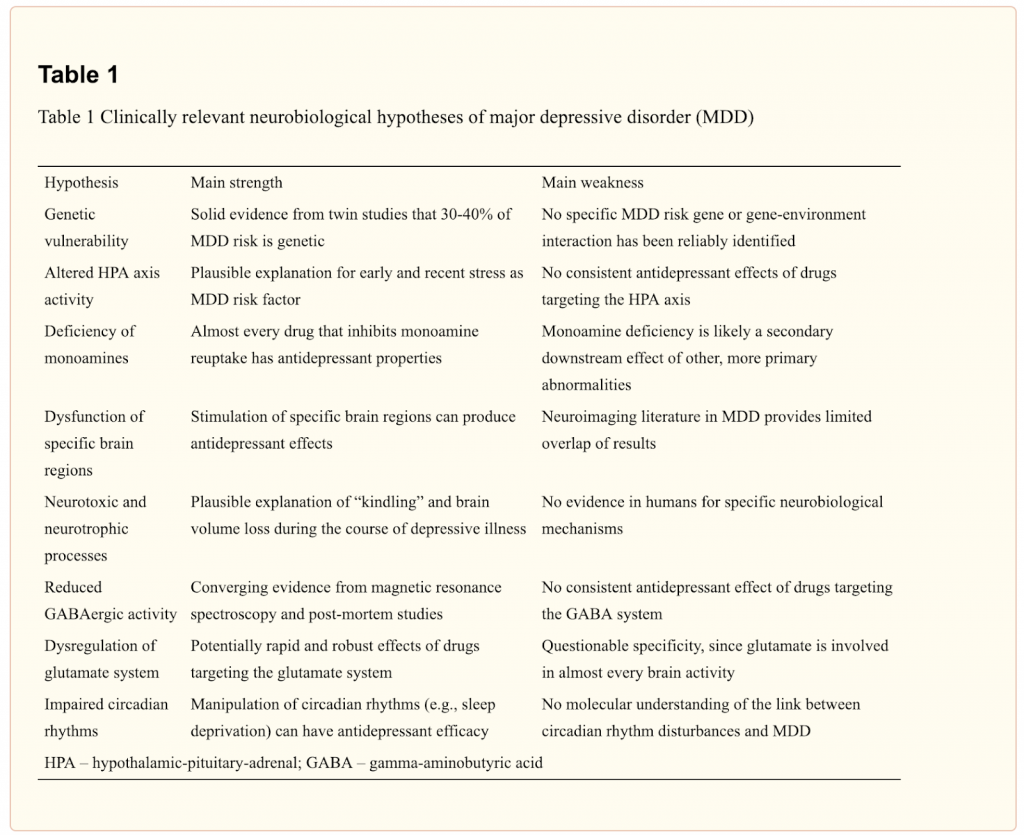
To borrow from a Buddhist parable: One can remove an arrow without knowing the name of the man who carved its shaft or the bird from which its feathers were taken.
We can also effectively treat depression without knowing one model that perfectly explains why it happens.
Do Conventional Antidepressants Work?
Even though the monoamine hypothesis has been largely rejected, numerous double blinded human studies suggest that SSRIs can treat depression better than placebo.
In conventional medicine, SSRI medications remain the first line of treatment for depression of all levels of severity.
Yet, problems maintain.
Irving Kirsh is a psychologist with an area of interest around the placebo phenomenon. He and a colleague were reviewing the literature on depression treatment because he was aware that there was often a robust placebo response with many treatments.
He was not interested in evaluating the efficacy of antidepressants – in fact, he assumed they were effective.
In his words:
“As a psychotherapist, I sometimes referred my severely depressed clients for prescriptions of antidepressant drugs.
“Sometimes the condition of my clients improved when they began taking antidepressants; sometimes it did not.
“When it did, I assumed it was the effect of the drug that was making them better.
“Given my long-standing interest in the placebo effect, I should have known better, but back then I did not.”46
The Placebo Effect
As he reviewed the studies, he was alarmed at how large the placebo effect was and how close it was to the efficacy of the medication.
In the majority of the studies, he found the differences were of only a few percentage points.
To see if this finding was legitimate, he requested a wider range of studies to evaluate. This next batch included many studies that were completed but were not used in the drug approval process.
What he learned was that pharmaceutical manufacturers did large numbers of studies that were not shared publicly. These studies were ones in which the medications did not work as well as placebos.
Key Insight: Altogether, 43% of the studies showed that the drugs worked, 57% showed that they did not work.
The degree by which the medications seemed to work in the positive studies was also extremely small. The tool used to evaluate their effectiveness was a 17 item depression survey called the HAM-D test.
The scoring ranged from 0-53 points. The effective studies showed that the score improved by 1.8 – 2.0 points. Medical groups considered changes of under 3 points to be statistically insignificant.
Did the Pills Work Even a Little Bit?
Maybe they did work, but a small amount and perhaps in some people the results could be more dramatic.
The problem with this theory is a concept called ‘broken blind.’ A difficulty with double-blinded studies can come up when the active medications cause side effects.
Participants who experience side effects often realize that they are on active medication and ‘break the blind’ portion of the study.
Since they know they are on active medication, they are even more likely to have placebo responses since their expectations are higher.
In one study, 89% of those on the active pill correctly guessed they were taking it due to the side effects they observed.
Once the ‘broken blind’ phenomenon and the unsubmitted studies are taken into consideration, the effectiveness of SSRIs on depression is exactly the same as placebo.47
What’s the Harm if They Seem to Help?
Again, in the context of a caring encounter with a credible and confident clinician, they likely do work, but not because of the chemistry of the medication.
Why not just use them as placebos? They are not harmless. In fact, they have been shown to increase the risk of suicide, stroke, and death from all causes.
It is not safe for pregnant women and have been shown to cause autism and birth defects in their offspring.
One of the most compelling reasons not to use them is that they INCREASE the risk of recurrent depression in all age groups that use them. Those who use them are more likely to be depressed in the future than those who do not.48,49
What if You are Already On Antidepressants?
Even if they seem to have been helpful, they are not intended for long term use. You cannot just quit taking them. You need to taper them under a doctor’s guidance.
Natural Antidepressants
The serotonin hypothesis has also inspired numerous natural treatments thought to treat depression via their effects on serotonin. The logic is that since serotonin is made from the precursor 5 hydroxytryptophan (5HTP) or from dietary tryptophan.50
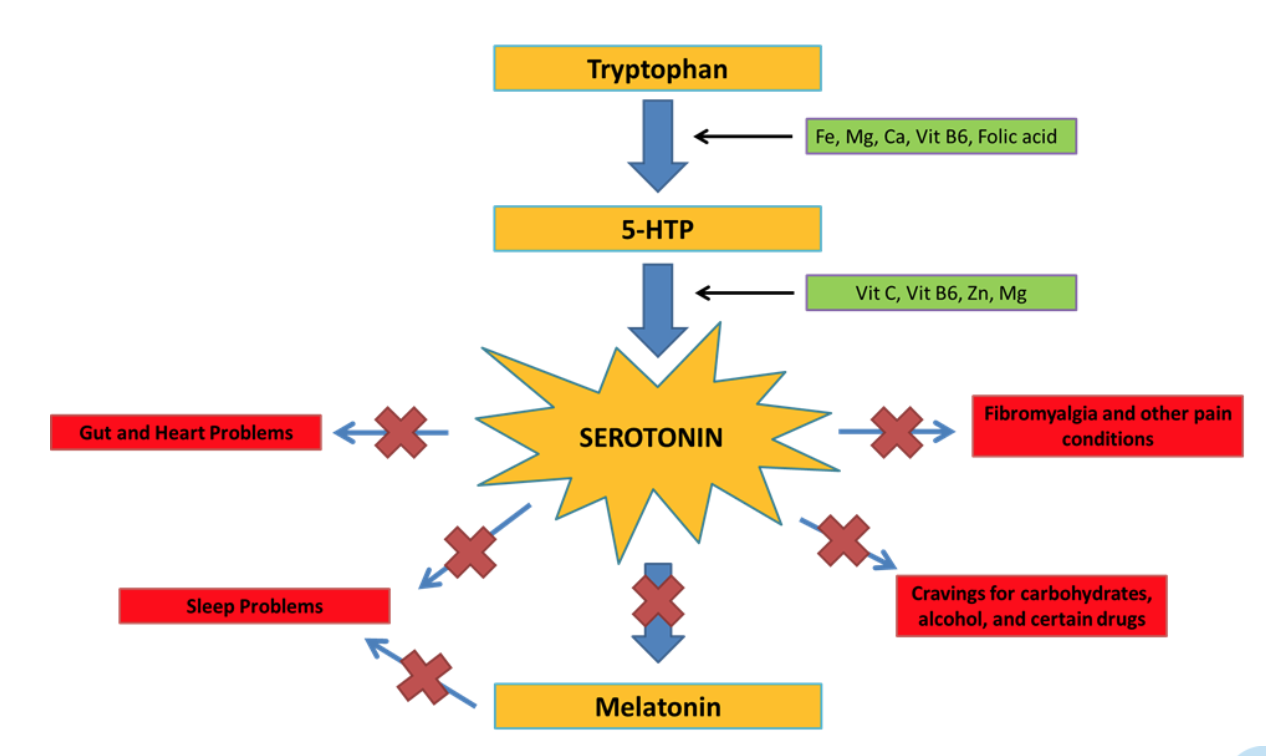
This basic idea is that if low serotonin is the cause of symptoms, massive doses of the building blocks for serotonin would raise serotonin and reverse the symptoms.
Again, this idea was studied in the late 1960s and found not to work. Nonetheless the myth has not yet died and in fact, many in natural medicine have doubled down and claimed that higher doses are needed and that in addition to serotonin precursors, amino acid precursors to other neurotransmitters must be included.
I call this the ‘key mistake.’ there are numerous examples where chemical reactions cannot occur without adequate amounts of an essential molecule as is true for 5HTP and serotonin. If 5HTP is lacking, serotonin cannot be made.
Think of 5HTP like a key for the car. Without it, the car cannot even move.
However, it does not stand to reason that the more 5HTP that a person ingests the more serotonin they will make.
Without the key, your car will not go. But once you have your key, more keys won’t make your car go any faster.
To date, no high-quality controlled human studies have shown that 5HTP or tryptophan supplementation can improve depression more than would be expected by a placebo response.51 Given that the serotonin hypothesis has failed, this is not surprising.
There is some evidence that oral 5HTP may slow cognitive tasks and due to serotonin formation in the intestinal tract, 5HTP may often cause gastrointestinal side effects.52
Putting It All Together
Here are some ideas to consider when creating your path to recovery. I put the steps in order, but you do not have to complete one before moving on to the others.
Please do not ignore any of them, but I would encourage you to start with at least a few suggestions from each step.
Depression happens for reasons and there are few cases in which people have just one cause.
There is usually something stressing the brain chemically, some life circumstances that are not ideal, and a bad relationship taking place between the person and his or her thoughts.
Step 1: Check the Medical Factors
Give the above discussion serious thought. In my experience, the vast majority of people with depression have at least one medical factor to consider.
For some it is the sole source of their symptoms, for others, it is at least a contributor. Until any hidden health factors are identified, the other steps will not work as well.
To get clear on your diagnosis, work with an excellent Naturopathic physician with conventional diagnostic skills or an excellent Naturopathic physician and a reputable local internist.
Step 2: Dial In Your Habits
On a typical day, aim to:
-
- Get 7 1/2 hours or more of good quality sleep
- Spend time in nature
- Eat seafood53
- Spend time with friends
- Work up to about an hour of intense aerobic exercise most days
- Take 1 gram of fish oil (already in your Daily Reset Pack)
Key Insight: Which of those are you doing great on? Be sure to keep that up. Which has the most room for improvement? That is your best immediate focus.
Step 3: Check In On Your Life
Ask yourself these questions:
- Have fulfilling work or hobbies?
- Enjoy close relationships with family, a romantic partner, friends, co-workers?
- Live in a safe area?
- Have easy access to nature?
- Find your home and neighborhood aesthetically pleasing?
- On conversational terms with your neighbors?
These items are not ones that can be changed abruptly. Thankfully you don’t have to have them all perfect in order to feel better.
Identifying those that could serve you more and starting on a plan to correct them is all that it takes.
Step 4: Question Your Thoughts
Have you done much training in Cognitive Behavioural Therapy, Mindfulness Meditation, or Acceptance and Commitment Therapy?
For mild depression, explore books, apps, or online programs for the above. Some of my top recommendations include:
- Mindfulness (App – Waking up with Sam Harris)
- ACT (Book – The Happiness Trap by Russ Harris)
- CBT (Workbook – Retrain Your Brain: Cognitive Behavioral Therapy in 7 Weeks: A Workbook for Managing Depression and Anxiety)
For moderate or severe depression, start with ACT or CBT with a licensed practitioner. Working with someone remotely is a reasonable option but in-person care may be best for those with the most significant symptoms.
Bottom Line: These therapies work because they can improve your relationship with your thoughts. It turns out that those who are depressed don’t have more negative thoughts than others, but they take more of their thoughts at face value.
If someone feels bad about feeling bad they can easily create a loop that can cause a passing thought to become a lasting emotional state.
Ironically the evidence is clear that we cannot change our thoughts.
Whatever you do, stick with it and expect 4-6 weeks to see an effect. It really works best to follow up with a health practitioner to help judge your progress. It is hard to be objective about gradual changes to ourselves.
Your Long-Term Outlook
The human mind is prone to depression, and situations that trigger it are normal occurrences in life.
However, those who have successfully resolved depression by addressing all of the above steps will be more capable of staying stable.
They will also be more able to be the necessary anchor to help loved ones through times of crisis. Just know: you can feel better. I hope you can get started to help optimize your health today (Click Here).
Resources
1 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC486942/
2 – https://www.ncbi.nlm.nih.gov/pubmed/17900039
3 – https://www.amazon.com/Happiness-Trap-Struggling-Start-Living/dp/1590305841
4 – https://health.howstuffworks.com/mental-health/depression
5 – https://www.apa.org/monitor/2019/01/gen-z
6 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2950973/
7 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2950973/#B11
8 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5409906/
9 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5541277/
10 – https://www.jstage.jst.go.jp/article/endocrj/64/4/64_EJ16-0418/_pdf/-char/en
11 – https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-017-1478-9
12 – https://www.ncbi.nlm.nih.gov/pubmed/22285302
13 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3019023/
14 – https://www.ncbi.nlm.nih.gov/m/pubmed/26580313/
15 – https://sci-hub.tw/10.1016/j.jpsychires.2016.02.023#
16 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6087692/
17 – https://www.wjgnet.com/2220-3206/full/v8/i3/97.htm
18 – https://www.sciencedirect.com/science/article/pii/S0165178117301981
19 – https://www.ncbi.nlm.nih.gov/pubmed/30184533
20 – https://www.ncbi.nlm.nih.gov/pubmed/573061
21 – https://www.ncbi.nlm.nih.gov/pubmed/21349213
22 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4826990/
23 – https://www.ncbi.nlm.nih.gov/pubmed/30791349
24 – https://www.ncbi.nlm.nih.gov/pubmed/21382111
25 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3765610/
26 – https://www.ncbi.nlm.nih.gov/pubmed/26997174
27 – https://www.ncbi.nlm.nih.gov/pubmed/21890213
28 – https://sci-hub.tw/10.1188/19.CJON.131-134#
29 – https://www.bmj.com/content/347/bmj.f4913
30 – https://positivepsychologyprogram.com/cbt/
31 – https://sci-hub.tw/10.1016/j.jpsychores.2017.12.012#
32 – https://www.ncbi.nlm.nih.gov/pubmed/29080598
33 – https://www.ncbi.nlm.nih.gov/pubmed/27479642
34 – https://www.ncbi.nlm.nih.gov/pubmed/28271287
35 – https://www.ncbi.nlm.nih.gov/pubmed/30656813
36 – https://www.apa.org/monitor/2015/03/cover-mindfulness
37 – https://www.webmd.com/depression/features/antidepressant-effects#1
38 – https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0020392#pmed-0020392-b6
39 – https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0020392#pmed-0020392-b7
40 – https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0020392
41 – https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0020392#pmed-0020392-b11
42 – https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0020392#pmed-0020392-b17
43 – https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0020392#pmed-0020392-b24
44 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2950973/
45 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2950973/table/T1/?report=objectonly
46 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4172306/
47 – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4172306/
48 – https://www.ncbi.nlm.nih.gov/pubmed/18540740/
49 – https://www.ncbi.nlm.nih.gov/pubmed/22536191/
50 – https://bebrainfit.com/5-htp-supplements-anxiety-depression/
51 – https://www.ncbi.nlm.nih.gov/pubmed/11869656
52 – https://www.ncbi.nlm.nih.gov/pubmed/23609610
53 – https://jech.bmj.com/content/70/3/299
1. Schedule a Thyroid Second Opinion with me, Dr. C, Click Here for Details
2. Download and use my Favorite Recipes Cookbook Here
3. Check out my podcast Medical Myths, Legends, and Fairytales Here
Dr. Alan Glen Christianson (Dr. C) is a Naturopathic Endocrinologist and the author of The NY Times bestselling Adrenal Reset Diet, The Metabolism Reset Diet and The Thyroid Reset Diet.
Dr. C’s gift for figuring out what really works has helped hundreds of thousands of people reverse thyroid disease, lose weight, diabetes, and regain energy. Learn more about the surprising story that started his quest.


